Background
This nonprofit health benefits company is focused on improving the health and lives of its one million members. It is nationally recognized in the United States as a leader for quality, customer service, transparency, and product innovation. As the fastest-growing healthcare plan in the state in which it operates, it is accepted by the majority of hospitals and primary care providers in its state. The healthcare company is committed to the community and focused on low overhead, cost savings, and personalized support, while offering a broad range of individual, family, small business, and large group plans. They also provide services to Medicare beneficiaries, placing a high priority on ensuring senior citizens receive responsive customer service that yields consistently high customer satisfaction rates.
The Challenge
The state health plan is committed to providing excellent customer service. Their internal agents deliver inbound and outbound customer care to the plan’s one million members. Determined to reach their average speed of answer (ASA) goals, they found they needed additional support to meet seasonal open enrollment demands and to help elderly Medicare customers get back on track when facing hardships.
They needed more cost-effective solutions to be able to ramp effectively with sufficient staffing levels of full-time employees (FTEs) during open enrollment. They also needed to ensure these employees were trained quickly and effectively with in-depth knowledge to provide personalized care to customers from a wide variety of backgrounds in an empathetic, understanding way.
Additionally, they sought support for accounts receivable management (ARM) and for providing friendly reminders and solutions to help elderly customers retain their Medicare services when in the midst of hardship. The focus was on keeping customers satisfied and providing compassionate service responsive to their needs.
All in all, the company is in it for the long haul—they want to keep their customers for life and they know that hinges on providing excellent customer experiences with 100% satisfaction rates.
The Solution
iQor began working with the healthcare benefits company in 2012 with a team dedicated to providing empathetic outbound accounts receivable management support to help Medicare customers get back on track. The demographics of the customer service agents differed significantly from those of the customers they served. In order to provide the best customer service experiences, the agents needed to understand their customers’ needs. To this end, the iQor team proactively developed a multifaceted program to help agents understand and connect with older customers.
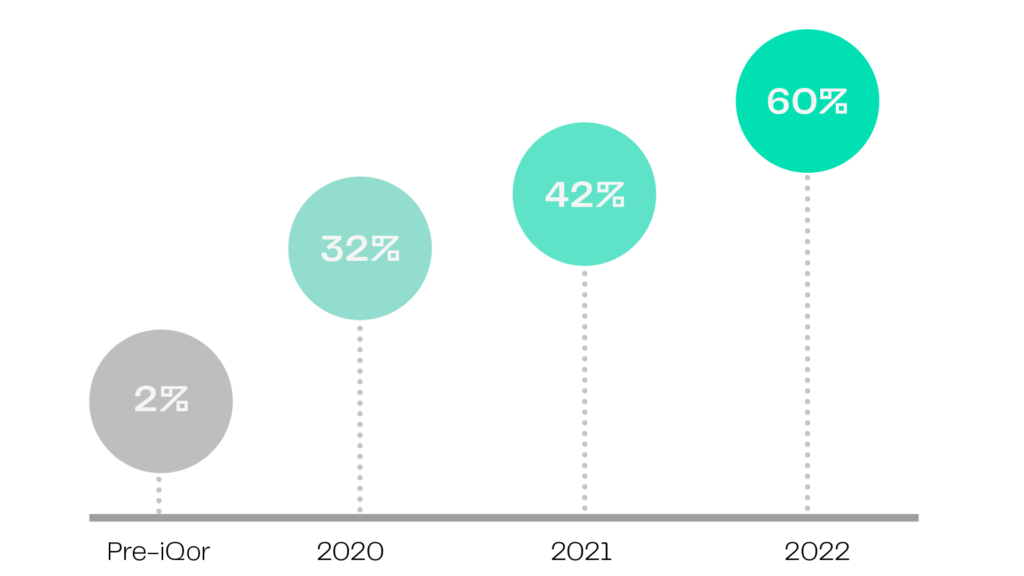
This approach yielded great success. After piloting outbound customer support for a year and consistently exceeding the healthcare benefits company’s expectations, iQor gained their trust as a valued partner in their customer service offerings. As a result, iQor transitioned to providing inbound customer support at a steady state and supporting seasonal ramps. This was the first time the healthcare benefits company had outsourced inbound customer service; iQor remains their only business process outsourcing (BPO) partner to this day. iQor provides inbound customer care on multiple lines of business with a steady state of FTEs that increases to more than 100 during open enrollment.
Implemented In-Depth Training
iQor created an intensive six-week training program to develop agents, focusing on complex content knowledge, compliance, and empathetic and personalized service. iQor excelled at training agents not only for steady state service needs, but also for peak-season ramps that required training more than 5x the number of agents so they could become experts. iQor exceeded the healthcare benefits company’s requirements for performance and did so at a lower cost than they could provide internally.
Established Frequent and Open Communication With the Client
Weekly and bi-weekly meetings with the healthcare benefits company provided an ongoing detailed analysis of operations, goals, and achievements. These meetings solidified iQor as a trusted partner in the healthcare benefits company’s success.
Created a Unique Community Outreach Program
In line with iQorian Values focused on giving back to the community and a commitment to truly understanding customer needs, iQor’s program leadership reached out to local nursing homes and senior centers so customer service teams could build relationships with members of the community and better understand their needs. Teams regularly participated in resident programs such as bingo, seasonal activities, dances, arts and crafts, and more. These partnerships heightened agent awareness of circumstances customers may be encountering and created opportunities for staff to learn firsthand about consumer struggles and needs. These activities built empathy and patience, showing agents why, for example, it may take longer to handle a customer call—plus they created long-lasting bonds for both parties.
Shifted the Customer Interaction Focus Away From Being Time-Sensitive and Toward Building Caring Relationships
Because of the elderly customer demographic, KPIs like average handle time (AHT) were less important. Instead, customer service agents needed to talk to the consumer slowly and perhaps loudly so they could fully understand and appreciate the service and solutions being provided. Agents learned to take their time with customers, in part because they may be the only person the customer talks to that day. Program agents were also trained to understand the individual and unique challenges many of the consumers may be facing, including heart conditions or arthritis that could impact the speed of their interactions or how challenging it may be to hold the phone or write notes.
Implemented a Focus on True, Meaningful Customer Service and Compliance
The iQor team covered all angles of training and ongoing coaching to ensure agents were equipped to provide personalized, empathetic service to a niche customer base. The teams also placed a high level of importance on compliance, ensuring all endpoint security measures, training, government regulations, and healthcare guidelines were followed.
The Results
iQor implemented a budget-friendly, results-focused customer-care solution that included weekly and bi-weekly touch-bases with the client. The iQor team worked closely with the healthcare benefits company to ensure high levels of customer satisfaction and to establish procedures for following up with customers that may need additional support.
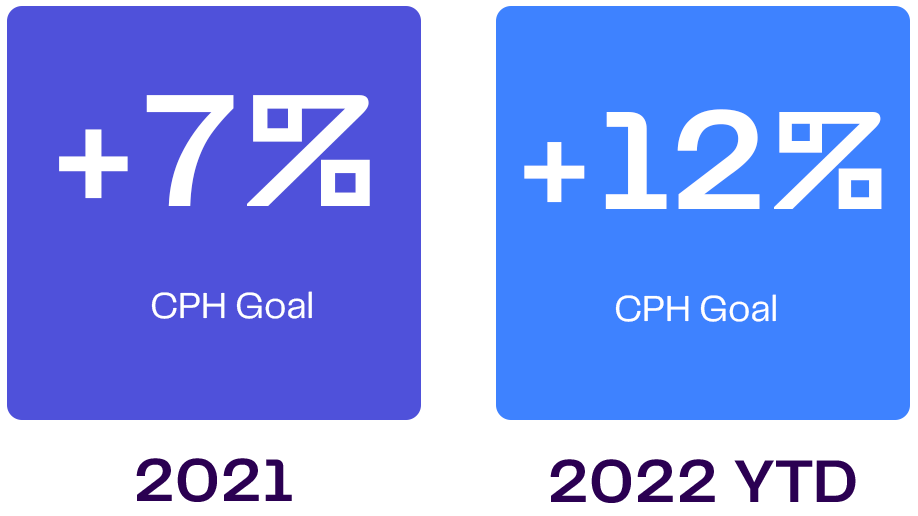
iQor’s actions resulted in improved scores that met and exceeded operational goals. The KPIs for the different lines of business reflect differing results based on the needs of the customers for each program.

Expanded Engagements With Nearly Identical AHT
Total call volume jumped 45% from 40,000 to 58,000 while AHT stayed nearly constant, demonstrating consistent support.

Exceeded Medicare Quality Score Goals
The program team generated a 1% improvement in the Medicare Quality Score.

Excelled at High Quality Ratings
The team supporting the individual plan surpassed the quality experience goal by 7% and the quality technical goal by 8%.
While the metrics matter, there’s one true measure of overall success: client and customer satisfaction. iQor has provided exceptional service and earned its place as a loyal and trusted partner of the healthcare benefits client for more than a decade. iQor teams are truly committed to providing exceptional service that makes employees and customers smile.